A few good rapidly prototyping images I identified:
The Race to Build a True-Life Version of the “Star Trek” Tricorder

Image by genphyslab
The Race to Construct a Actual-Life Version of the “Star Trek” Tricorder – General PHYSICS LABORATORY (GPL)
By Evan Ackerman
Photo: XPRIZETech From “Star Trek” Dressed in a Starfleet uniform, Tatiana Rypinski holds a replica tricorder for the duration of a photo shoot for the Qualcomm Tricorder XPrize. She leads a single of the finalist teams in the competitors.
Tatiana Rypinski is maybe two bites into her salad when she realizes it’s time for her next meeting. She gets to her feet and heads to the Biomedical Engineering Design and style Studio, a hybrid of prototyping space, wet lab, and machine shop at the Johns Hopkins University’s Homewood campus, in Baltimore. Rypinski and a couple of of her colleagues collect close to some worktables with energy outlets dangling from the ceiling. A tool cart is in 1 corner, a microscope in one more. Two three-D printers sit idle along a wall. The students have agreed to meet me right here to discuss their perform on a project whose purpose is not just inspired by science fiction—it in fact comes straight out of “Star Trek.” They want to create a medical tricorder.
In 1966, “Star Trek” introduced the tricorder as, in essence, a plot device. Like the transporter, which could “beam” individuals in between starships and planets with no asking the audience to sit via lengthy landing sequences, the tricorder could quickly diagnose healthcare circumstances and recommend treatment options, keeping the story moving. With a wave of this fictional device, a Starfleet crew member could get a complete health-related evaluation with no possessing to be admitted to the ship’s sick bay.
Right here in the true globe, although, if you have a nonemergency scenario, you may wait days—weeks, in some places—to see a doctor. And if you want laboratory tests, receiving a diagnosis can take even longer. A lot of waiting is involved, and waiting is the final factor you want to do when you’re sick. It’s even worse in the building world, where a shortage of health-related facilities and personnel implies that seeing a physician may not be an alternative at all. What we need to have is a tricorder. A genuine a single.
Rypinski is the leader of Aezon, one of the teams participating in the Qualcomm Tricorder XPrize. The competition launched in 2012, when the XPrize Foundation and U.S. chipmaker Qualcomm challenged innovators from about the planet to create a portable, consumer-friendly device capable of diagnosing a complete set of health-related circumstances. A lot more than 300 teams registered, and soon after a series of critiques, the organizers selected 10 finalists, announced last August.
This month, the final phase of the competition begins. Each and every finalist team was expected to deliver 30 working prototypes, which will now undergo a battery of tests with genuine patients. Prizes totaling US million will go to the winner and two runners-up, to be announced early subsequent year, when “Star Trek” will be celebrating its 50th anniversary.
Aezon is the youngest finalist team: All of its members are undergraduates at Hopkins. Some have by no means even observed the original “Star Trek” episodes. “My dad is a huge fan, even though,” a single student tells me. For her component, Rypinski is unfazed. “This is anything we’re doing because we love it,” she says, “and I feel that sets us apart.”
The other finalists contain high-profile startups like Scanadu, in Silicon Valley, and properly-funded health-related organizations like DNA Medicine Institute, in Cambridge, Mass., which has a partnership with NASA. 4 teams are based in the United States, and the other six are from Canada, England, India, Northern Ireland, Slovenia, and Taiwan.
Their tricorders won’t be all-powerful transportable scanners like these in “Star Trek,” but they nevertheless must demonstrate some impressive capabilities. They’ll have to diagnose 13 medical circumstances, like anemia, diabetes, hepatitis A, leukocytosis, pneumonia, stroke, tuberculosis, and urinary tract infections. In addition, teams pick three further conditions from a list that includes meals-borne illness, melanoma, osteoporosis, whooping cough, shingles, mononucleosis, strep throat, and HIV. And their systems must be capable to monitor important indicators like temperature, blood stress and oxygen saturation, heart price, and respiratory rate—not only in true time but for periods of many days as properly.
The objectives might appear impossibly hard, but XPrize believes they can be achieved, thanks to a host of fairly recent technological advances. These incorporate sophisticated machine-studying approaches applied to health-related data, price-powerful microfluidic and other lab-on-a-chip systems, and faster and more affordable laboratory tests such as rapid polymerase chain reaction (PCR) for DNA evaluation. Just as critical, there’s the popularization of individual genomics services and fitness-tracking gear, exemplifying people’s need to find out more about their bodies and health.
Simply because the enabling technologies currently exist in some kind right now, a lot of the challenge is about integrating them into a compelling program, says Grant Campany, senior director of the Qualcomm Tricorder XPrize. A tricorder isn’t intended to maintain you out of your physician’s office: It won’t be capable to treat any of the situations it can identify. But it will be capable to give you a quick and detailed image of what may possibly be the matter with you—which is significantly better than googling your symptoms and sorting via dubious medical sites, as numerous people do today.
Campany says the diseases chosen for the challenge are often not diagnosed early adequate and for that reason lead to a substantial quantity of deaths and hospitalizations: “The purpose here is to attempt to identify things as soon as possible so that men and women don’t wait and get sicker.”
Tricorder XPrize: The Final Frontier
This month, the US million Qualcomm Tricorder XPrize enters its final phase. The ten finalists listed beneath are expected to deliver a set of working prototypes to be tested with genuine sufferers. The winner will be announced early next year.
Aezon (Rockville, Md.)
Students from Johns Hopkins University are creating a 3-element program that consists of a smartphone app, a vitals monitoring device worn about the neck, and a lab unit to analyze samples of blood, urine, and saliva.
Cloud DX (Kitchener, Ont., Canada)
The private business’s dozen or so engineers and scientists are creating Vitaliti, a vitals monitor worn about the neck. The group’s tricorder will also include an earpiece and lab evaluation unit with smartphone integration.
Danvantri (Chennai, India)
Backed by technology firm American Megatrends India, Danvantri (named for the Hindu god of medicine) is augmenting its commercially offered B.OL.T. electronic blood stress cuff with a suite of modular sensors for its tricorder.
DMI (Cambridge, Mass.)
DMI plans to integrate its advanced diagnostic technique (which won XPrize’s Nokia Sensing XChallenge in 2014 and will undergo trials on the International Space Station) with a wearable vitals patch.
Dynamical Biomarkers Group (Zhongli City, Taiwan)
Sponsored by smartphone manufacturer HTC, DBG is a group of Taiwanese and U.S. engineers and physicians. It is constructing a tricorder based on a sensor suite and imaging technique to analyze vitals and samples of blood and urine.
Final Frontier Health-related Devices (Paoli, Pa.)
Three brothers and a sister—with backgrounds in medicine, engineering, and personal computer science—form the core of Final Frontier. Their tricorder contains a handheld device that utilizes optical sensors to avoid the require for blood samples.
MESI Simplifying Diagnostics (Ljubljana, Slovenia)
MESI is a startup founded by a group of physicians and engineers. Its tricorder consists of a health-related-grade wristband, a smartphone app, and a couple of diagnostic modules for identification of distinct illnesses.
Scanadu (Moffett Field, Calif.)
With Scout, a handheld vitals scanner, Scanadu reached a record .six million in crowdsourced funding in 2013. For its XPrize tricorder, the team could enhance Scout and combine it with a wearable device and a lab test kit.
SCANurse (London)
A diagnostic medical manufacturer, SCANurse is hoping to develop a tricorder that is “minimally invasive,” employing sensors and laptop vision whenever feasible alternatively of asking patients to supply blood or urine.
Zensor (Belfast, Northern Ireland)
The team is focusing on a wearable electrocardiogram sensor that also measures vitals like respiration rate and temperature. Diagnostics on blood and urine will be performed by a miniature microspectroscopy lab.
It’s late February, and Aezon is reaching a critical phase of its project. Rypinski tells me the team has a number of operating components but now requirements to combine them into a total method that can be delivered to the organizers in just 3 months. There’s a restricted amount that she’s prepared to share with me about her group’s tricorder Aezon, like most other XPrize competitors, is maintaining its technologies heavily under wraps.
Nevertheless, it’s secure to say the a variety of systems will most likely work in a comparable style. How? Say you’re feeling ill. Most tricorders will probably consist of an application running on a telephone or tablet as the main user interface. The app—a sort of AI doctor—will start by asking you a series of inquiries: Do you have a headache? Are you feeling dizzy? Did you vomit? It could also ask you about your age, weight, height, and healthcare history.
Next, it will collect your vitals, measured by a sensing device you wear on your body—a fitness tracker–style wristband, or possibly an electronic necklace. (The competitors calls for this monitor to be in a position to collect data for 72 hours, even whilst you sleep.) Based on your answers and essential signs, the app could ask you to perform some added tests. These you will do making use of yet one more piece of hardware, a type of “lab in a box” unit, which will be in a position to perform certain diagnostic tests utilizing samples of saliva, urine, or blood.
Finally, soon after getting the test results and crunching all the other information, the app will give you a diagnosis and direct you to more details such as dependable medical resources or help groups for individuals with that illness. It may also include a “call your doctor” button, or it may even dial an emergency quantity.
Some teams are building devices that you could error for a “Star Trek” prop. Scanadu, before it joined the XPrize competitors, ran a extremely profitable crowdfunding campaign to develop Scout, a sleek white disc you place against your forehead. Packed with sensors, the little device measures heart rate, skin and core physique temperature, respiration rate, blood pressure and oxygen saturation, and electrocardiogram (ECG) information. For the XPrize, it’s unclear regardless of whether the company will use the exact same device or improve it, perhaps coupling it with a wearable accessory that can collect information over longer periods.
Canadian group Cloud DX has designed a futuristic-hunting plastic collar to measure vital signs. The U-shaped device wraps about your neck, and its extremities have electrodes that sit over your chest to record your heart’s electrical activity. Its tricorder also consists of a lipstick-size scanning wand for skin and ear exams that its creators say “Dr. McCoy would be proud of,” referring to the USS
Enterprise‘s chief healthcare officer.
Sitting in the Biomedical
Engineering Style Studio, Rypinski and her colleagues appear definitely exhausted, and it seems like they’re operating on small much more than determined enthusiasm. She tells me that following reading about the tricorder competitors in 2012, she sent e-mails to various departments at Johns Hopkins—known for its powerful biomedical engineering program—to see if anybody was interested in forming a team. A lot of men and women showed up for the 1st handful of meetings. The difficult component was finding individuals who would come back. “Over time, the folks who had been truly interested in the project stuck with it,” she says, “and right here we are.”
For the competitors, Aezon adopted a divide-and-conquer strategy. The 30 or so group members formed tiny groups to investigate person ailments and establish which information they needed to effectively diagnose every of them.
Two of Rypinski’s colleagues—Alex Kearns, a mechanical engineering student, and Akshay Srivatsan, a laptop science student—tell me they have developed a smartphone-based diagnostic app that operates “the way a medical doctor thinks.” To do that, the app relies on a machine-learning approach known as a naive Bayes classifier, which is commonly employed by researchers developing such healthcare-diagnostic applications. The concept is to adjust the probability of a given diagnosis every single time the method receives a new piece of data, which may possibly consist of symptoms, vitals, or lab benefits.
To collect important signs from individuals, some Aezon group members created a monitoring device to be worn around the neck. Its creators decided to kind an independent firm, Aegle, to raise funds and market the monitor separately following the competitors.
For some of its tests, Aezon has partnered with the Johns Hopkins BioMEMS & Single Molecule Dynamics Lab. The group is hoping that some micro- and nanoscale molecular analysis methods not too long ago created at the lab could be employed in a quickly and low-cost diagnostic test of blood samples.
For other tests, though, the group is turning to simpler technologies. Cyrus Zhou, a biophysics key, and Ned Samson, a mechanical engineering student, are operating on a test for leukocytosis, which is an elevated white blood cell count. “Initially, we had been going to make a microfluidic device,” says Samson. “But from the folks we talked to, it’s like a Ph.D. to do that.”
The students found a commercially available chip that causes blood cells to spread out, creating them easier to see. They’re now trying to combine the chip with a set of lenses that can act as a easy and affordable optical microscope. Their plan is to use the camera on the smartphone and Aezon’s app to count white blood cells with laptop vision. “It’s got every little thing,” says Samson. “It’s small, it’s expense effective, it’s doable.”
Between June and December of this year, XPrize will assess the teams’ prototypes at the UC San Diego Medical Center. The effort will involve recruiting nearly 500 people—three customer testers per device, per condition—to acquire a representative outcome for every condition with each tricorder.
The winning team will be the one particular that has the highest health assessment score (primarily based on the tricorder’s potential to correctly identify the condition that the user has) while also getting among the five teams with the highest “consumer experience” score (primarily based on the tricorder’s aesthetic appeal, ease of use, and functionality).
“These devices must be in a position to function in such a way that a typical individual with some understanding of smartphones ought to be capable to understand how to operate them,” says Campany, the Tricorder XPrize director. “We’ve put 45 % of the score on the consumer expertise, since that’s how essential we think it is.”
This assessment won’t be a clinical trial, which would be far more challenging. Even if some of the tricorders operate nicely, there will still be a lengthy list of queries that will need to have to be answered prior to the devices can be commercialized. Are they safe? Do they keep a user’s medical information private? Who’s liable if there’s a misdiagnosis?
A month following my pay a visit to to Johns Hopkins, I verify in with Rypinski to see how items are going. Aezon has finalized the design of its tricorder and is now tweaking its elements to make positive they work nicely with each other and offer a cohesive user encounter. Rypinski doesn’t know how she will really feel when the prototype ultimately ships to XPrize—and there’s practically nothing far more that her team (or any of the other teams) can do, apart from wait for the benefits of the consumer testing. Proper now she can barely locate time to consume lunch.
“We have a really tight deadline to meet,” she says. “After that, we’ll have all the time in the planet.”
Tricorder stand-in
Your Smartphone
Can a smartphone tricked out with gizmos and apps replace a doctor’s classic diagnostic tools? We’ll quickly discover out. Capitalizing on the impressive sensors and processing energy in today’s smartphones, startups are turning them into mobile diagnostic and monitoring instruments for both consumers and health care workers. As capable as some of these innovations currently are, it’s unclear regardless of whether they will pass muster with government regulators, which is why many of their makers are not but touting them as bona fide medical devices. —Sarah Lewin
Pediatrics
Infant Essential-Indicators Checker
The Owlet Wise Sock keeps tabs on an infant’s heart rate and blood-oxygen levels. LEDs shine red and infrared light via the foot, and sensors measure how that light is absorbed by oxygen-carrying hemoglobin molecules in arterial blood. The sock transmits this information more than Bluetooth to a base station and to the smartphone of the nearby (and presumably anxious) parent.
Cost: US (offered for preorder)
Ophthalmology
Eye Examiner
The Transportable Eye Examination Kit (PEEK) adds a lens adapter to the smartphone’s camera. Overall health care workers in remote locations can then use the phone to scan a patient’s retina for disease and to verify for cataracts. Associated smartphone apps can be employed to test the patient’s vision.
Cost: £70 (accessible for preorder not available in the United States)
Otology
Eardrum Inspector
The Oto turns an iPhone into an otoscope that utilizes the phone’s camera to view the eardrum at high magnification. With the house version, parents can send photos of their youngsters’s eardrums to on-contact clinicians to diagnose middle-ear infections. A pro version allows medical doctors to share images with their individuals.
Price: US for the Oto Property (at present available only in California) 9 for the Oto Clinic
Cardiology
An ECG in Your Telephone
With the AliveCor Heart Monitor, a patient with a heart condition can gather a individual electrocardiogram, a record of the heart’s electrical activity. While the patient touches electrode-carrying sensors attached to the telephone’s case, an connected app displays the patient’s heart rate and flags irregular rhythms known as atrial fibrillations. The app also transmits information to the patient’s physician.
Value: US
Illustrations: James Provost
Psychology
One thing to Watch More than You
Mental-health clinicians can use the Mobile Therapy app to maintain tabs on individuals amongst sessions. The app makes use of self-reports, linguistic evaluation, and smartphone sensors to gather data about the patient’s feelings, behaviors, movements, and interactions with other men and women. It then relays this data to the clinician, who can appear for trends and spot problems signs.
Price: US per year for a clinician
This report originally appeared in print as “The Race to Build a Genuine-Life Tricorder.”
Share on Facebook (Opens in new window)Click to share on Twitter (Opens in new window)Click to share on Google+ (Opens in new window)A lot moreClick to share on Tumblr (Opens in new window)Click to share on LinkedIn (Opens in new window)Click to share on Pinterest (Opens in new window)Click to share on Reddit (Opens in new window)Click to share on Pocket (Opens in new window)Click to share on StumbleUpon (Opens in new window)Click to e mail this to a buddy (Opens in new window)Click to print (Opens in new window)
www.genphys.com/engineering/engineering-news/the-race-to-…
Internet Thingies
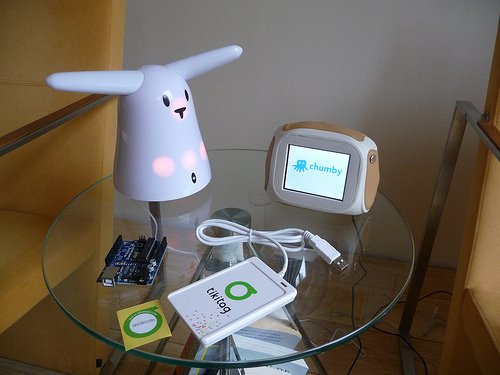
Image by TonZ
Experimental gadgets in our household about the ‘Internet of Things’